GRS Select™ — available now!
With our new, customizable revenue cycle offering you can choose the services your practice needs the most. Customize your plan

We have a solution for every challenge
Technology and services that seamlessly span the front office, clinic, and billing office that help you deliver exceptional care and meet business goals.

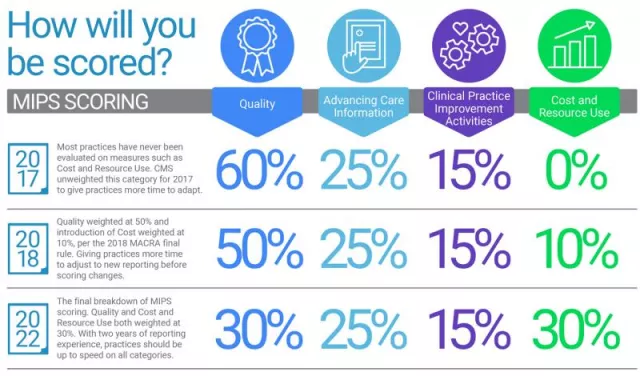
Our MACRA knowledge is at your fingertips


Brochure
Empowering FQHCs: Smart Technology for Stronger Community Health
Read More


Blog
How Greenway Health Advances Equity in Tribal and Urban Indian Healthcare
Read More


Benefit Overview
Enterprise Support Services Benefit Overview
Read More


Blog
Solving Healthcare's Silent Crisis: Why Provider Time Is the Most Valuable Resource in Medicine
Read More